Dialysis Patient Citizens (DPC) appreciates the opportunity to engage in ongoing dialogue and the continuous ability to provide feedback to the Centers for Medicare and Medicaid Services (CMS), Center for Medicare and Medicaid Innovation (CMMI) on issues related to the improvement of care for chronic disease (CKD) patients. In our July 23, 2012 letter to CMMI leadership, we proposed several initiatives to consider as integrated care projects are considered. To further enhance our earlier statements, we have included timely data from our nationwide survey of patients with end stage renal disease (ESRD).
For clarity, the following list includes the primary points from our earlier letter that suggested elements to include in any integrated nephrology care demonstration projects or pilot programs:
- Inclusion of patients at all stages of kidney disease, including those who are pre-dialysis, on dialysis and have transplants. With the number of patients with ESRD steadily increasing,innovation must be directed towards patients at all levels of kidney disease. Integrated care programs targeting pre-dialysis patients have the potential to shift care towards preventative therapies, slowing the progression to late state kidney disease, which in the long term can provide substantial cost savings. Any plan including opportunities for increased education will also help dialysis and transplant patients increase their compliance, reduce infections and hospitalizations as well as sustain transplanted organs. All patients deserve the opportunity to participate in innovative programs to improve their care.
- Provide incentives for primary care providers, dialysis clinic staff and nephrologists to participate in any new project. No matter how well developed a project is, it will not work unless all partners are willing to come to the table to change the way care is delivered. Allowing those tasked with improving patient care to share in these savings is a win-win model. Adapting practices to work within a new framework will require additional planning and resources. While many clinics already work in an integrated care framework, formalizing this relationship is a key step for longevity.
- Allow small/large, for-profit/non-profit provider organizations to participate in any demonstration/pilot project. Making any new integrated care project all inclusive from the start means more patients will be able to take advantage of the opportunities for better access to care and increase choice in services. If only larger providers are able to offer new projects,patients would have to travel farther to participate, and these providers would potentially gain competitive advantages.
- Build off of existing best practices to develop integrated care projects. Large and small providers have already done much of the leg work to create practices that improve patient care and substantially reduce costs. Groups have already adopted Accountable Care Organization (ACO) pseudo structures, created educational interventions and provided access to items such as nutritional supplements. Additionally, several successful demonstration projects have proven that these practices can improve patient outcomes. Now is the time to survey the landscape, speak with interested stakeholders and adapt successful practices into a nationwide pilot program.
- Utilize and maximize the time of dialysis therapies to provide education and other care interventions. Dialysis patients, especially those on in-center hemodialysis treatments, are in dialysis clinics or with providers more frequently than the general population. Choosing projects that take advantage of this opportunity will offer unprecedented time to provide education and potentially increase quality of care while reducing costs. Since kidney function affects many regions of the body and vice versa, CKD patients often have comorbid conditions. Having a guaranteed appointment for interventions enables medical teams to potentially treat beyond kidney disease.
DPC recently conducted an online and telephone survey that was sent to over 24,000 patient members and non-members. The survey is unique because it captures the patient perspective. Questions included a broad range of topics from drive times to anemia management and a complete section on nutrition. We wish to share a few data points that show the need for integrated care and the potential impact of demonstration projects or pilot programs.
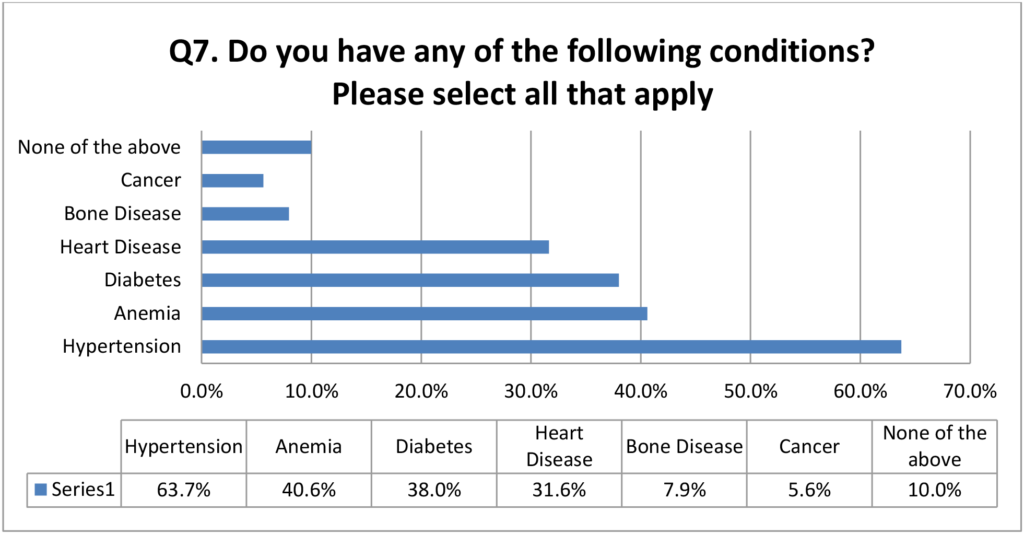
CKD patients often suffer from comorbidities, either causing their kidney disease or stemming from the disease itself. Our data in the chart below gives a visual representation of the patient population. Since there are high levels of concurrent disease, there is a large opportunity to create programs that not only help CKD patients, but also treat the body holistically to create lasting change. This is why CKD patients are an ideal group for a demonstration project and why it is imperative that as many providers and patients are eligible to participate.
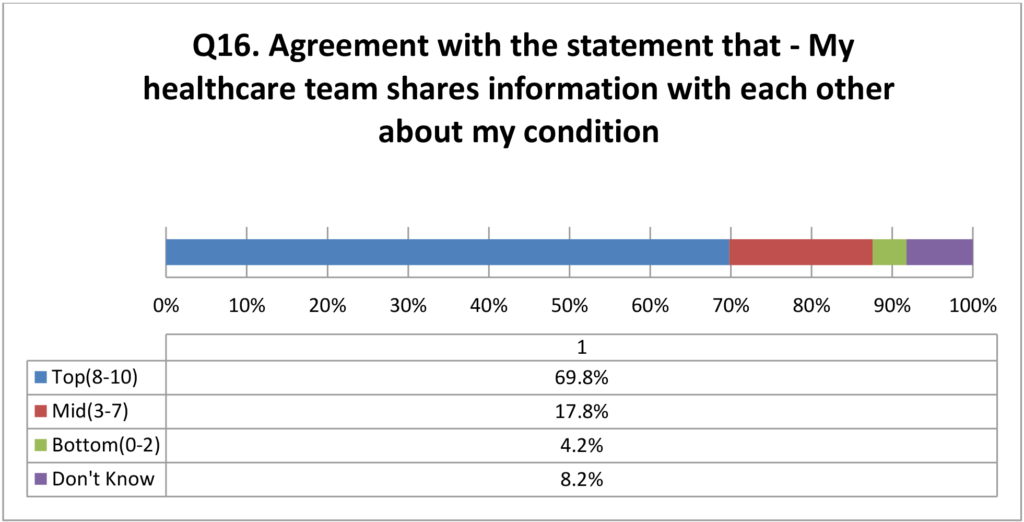
Patients also believe that their care providers (doctors, nurses, social workers, etc.) are already doing a good job of coordinating their care. When asked on a scale of 1-10 with 10 being the highest how well patients felt their providers shared their medical information, the overwhelming response was quite positive with a median score of 9.0. The figures in the chart below reinforces that currently care is being coordinated at clinics and it makes sense to formalize this relationship and encourage this behavior through incentives.
As CMMI leadership continues to listen to the renal community and define what integrated kidney care is, DPC looks forward to providing the patient perspective.
A final suggestion for inclusion in any new program is to determine measures of success for participating patients, such as treatment satisfaction, hospitalizations, and vascular accesses, to name a few. Additionally, there is a need to create control groups to measure improvements, and including pre-dialysis, dialysis and transplant patients would allow historical comparisons to groups before the new program is implemented and provide even more markers for success. We would be pleased to help determine patient metrics, when the time comes. Once again, we thank CMMI for the opportunity to provide feedback and for the aggressive push to improve patient care through innovation.