Before I was diagnosed with polycystic kidney disease while I was pregnant with my son, I knew nothing about kidney disease. I never would have imagined all the different things that go into treating it, and what it would eventually be like to go on dialysis.
Once I did start dialysis in 2016, I found myself in a whole different world. I remember just being overwhelmed learning about it all, and asking myself how I would possibly find a donor as I prepared each day for overnight dialysis treatments that lasted eight and a half hours.
What made things especially difficult was simply managing all of the appointments I had. Between my diagnostic workup appointment and my kidney transplant, I saw nephrologists, nurse practitioners, dieticians and even one geneticist, each of whom was responsible for a different part of my care.
While I did in-home treatments as long as I could, a nephrectomy caused me to have to do in-center treatments for two months while the surgical site healed, which only complicated things more since I was used to in-home treatment. This was especially true before I switched facilities from one near me in New Jersey, where I wasn’t comfortable, to one in Pennsylvania, as managing treatments at my old facility felt impossible at times.
The case is the same for so many dialysis patients across the country, and I hope Congress takes the opportunity to help. Legislators are working on the
BETTER Kidney Care Act, which would make coordinated care services more easily available for patients, meaning their various doctors and healthcare providers could more effectively communicate what treatments they’re giving, which medications they’re prescribing, and more. In the end, coordinated care means patients are spending less time in doctors’ offices and less money on treatments.
The BETTER Kidney Care Act also has other important provisions for dialysis patients, too. It has measures to help with travel for patients who don’t have a way to get to and from their dialysis clinics and also helps with dental care for patients, which is critical for hopeful transplant recipients.
The cost element in particular is significant. During my in-center dialysis treatments, I would be billed for every time I was there, and when I did in-home treatment, I was billed for each time I used my dialysis machine. It all quickly adds up since patients need dialysis treatments several times each week. Even with Medicare and my husband’s insurance, which was supposed to help make up for what Medicare didn’t cover, the costs were still a lot to handle, and I know that for the many patients who rely on Medicare for their treatments, the problem is even bigger.
That’s why it’s also important for Congress to pass the
Jack Reynolds Memorial Medigap Expansion Act, which can help patients manage costs by expanding the availability of Medigap coverage — coverage for the costs not paid by traditional Medicare — to dialysis patients under 65. Right now, those patients don’t always have access to Medigap coverage and get stuck paying for up to 20% of every dialysis treatment.
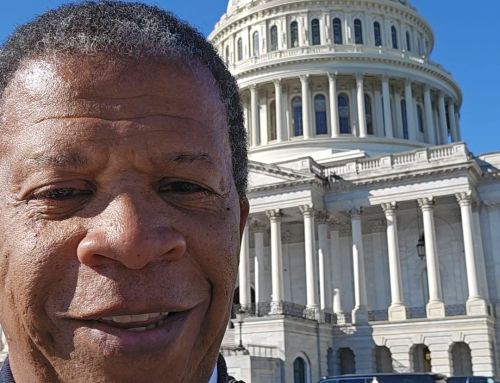
These are bills that I hope my representative, Congressman Donald Norcross, and his colleagues on Capitol Hill prioritize passing as soon as possible. Having done treatments at home in New Jersey and across the river in Philadelphia, I know care coordination and affordability are issues that affect patients in states across the country.
Too many patients are struggling with managing their care on their own, and the costs that come with it. Passing these bills can help to make a real, positive impact on kidney care in this country that makes the process easier and more affordable for patients.
One of the most important lessons I learned while I was going through dialysis and waiting for a transplant was that you have to do what you can to stay positive. Between the uncertainties over coordination, cost, and more, though, it can be tough. Congress has an opportunity to create a bit more certainty for dialysis patients, and I hope they do that by voting for these two crucial bills.
Ellyne Dombro, Cherry Hill, New Jersey