Dialysis Patient Citizens News
CMS-1651-P, Prospective Payment System and QIP
Andrew Slavitt, Acting Administrator Centers for Medicare and Medicaid Services Department of Health and Human Services Hubert H. Humphrey Building 200 Independence Avenue, SW Washington, D.C. 20201 Re: CMS-1651-P: End-Stage Renal Disease Prospective Payment System, Quality Incentive Program Dear Mr. Slavitt: Dialysis Patient Citizens (DPC) appreciates the opportunity to provide the Centers for Medicare and Medicaid Services (CMS) with comments on the proposed payment rule for the Medicare End Stage Renal Disease (ESRD) program. As America’s largest patient-led organization representing dialysis patients, DPC’s membership consists of more [...]
DPC Responds to CMS’ Request for Information
If anyone doesn’t know why the public is fed-up with our government, all they need to do is look at yesterday’s RFI on third party payment, which can best be summarized as “politics as usual” and big insurance dictating its own agenda. The former CMS Administrator – who is now the nation’s leading lobbyist for the insurance industry – appears to be getting the Agency to prioritize her new employer’s desires over the needs of the nation’s most vulnerable patients. To put even more pressure on the Obama Administration, Aetna just threatened [...]
Did Payment Reform Affect Patient Modality Choice?
One of the main policy goals of Dialysis Patient Citizens is to Improve Access to Care. This tenet includes improving patient access to all dialysis modalities: home hemodialysis, peritoneal dialysis, in-center hemodialysis and transplantation. Through our annual membership survey, we’ve uncovered various barriers for patients who would like to receive home hemodialysis. Many patients are unable to receive treatments in their home because of a lack of a caregiver, which is a requirement to receive treatment. However, DPC has also uncovered that the type of insurance a patient [...]
ESRD Choice Act Moves out of Committee with Unanimous Support
Dialysis Patient Citizens (DPC) hailed the introduction of H.R. 5659 as the latest in a series of milestones toward opening Medicare Advantage (MA) enrollment to end-stage renal disease (ESRD) patients. With bi-partisan introduction by Reps. Jason Smith (R-MO), John Lewis (D-GA), Gus Bilirakis (R-FL), Kurt Schrader (D-OR) and Tom Marino (R-PA), this legislation is a momentous step forward to providing dialysis patients increased access to insurance. “As a dialysis patient of 5 years, I am fortunate to have secondary insurance to cover what Medicare does not, however I know [...]
DPC Complaint to OFM re: Washington State Insurance Plans
Re: Violations of the Medicare Secondary Payer Statute, 42 U.S.C. § 1395y(b), by Washington State Health Insurance Plans Dear Ms. Parker and Ms. Dotzel: We write to bring to your attention the fact that at least three group insurers in the state of Washington are offering large plans with provisions that violate the explicit terms of the Medicare Secondary Payer Statute. These violations not only potentially subject the insurers to statutory civil monetary penalties, but render these insurers’ plans nonconforming under applicable regulations. As America's largest patient-led organization [...]
CMS Proposes Payment Updates for ESRD and New Policies for Quality Incentive Program (QIP)
Each year, the Centers for Medicare & Medicaid Services (CMS) issue proposed rules to update payment rates under the End-Stage Renal Disease (ESRD) Prospective Payment System (PPS) for renal dialysis services for the following year. On June 24, 2016, CMS proposed updates to the PPS as well as new quality measures for 2017. Notably, CMS proposed an increase to the base rate paid to dialysis facilities of $0.65 in addition to proposing increasing the home and self-dialysis training payment. In regards to quality measures, CMS proposes the inclusion of a new [...]
New Legislation Introduced to Improve Dialysis Patient Care
The Dialysis PATIENT Act (Patient Access To Integrated care, Empowerment, Nephrologists, and Treatment), S. 3090, recently introduced by Senators Heller (R-NV) and Nelson (D-FL). It follows introduction of the House version (H.R. 5506) the previous week by Reps. Young (R-IN), Blumenauer (D-OR), McMorris Rodgers (R-WA) and Cardenas (D-CA). The Dialysis PATIENT Act would permit dialysis organizations to accept capitated payments to cover all of an ESRD patient's Medicare expenditures in return for coordinating care for their renal disease and other comorbidities. The program would be voluntary for patients [...]
DPC Complaint to Department of Labor re: Insurance Plan Discrimination
The Honorable Phyllis C. Borzi Assistant Secretary Employee Benefits Security Administration United States Department of Labor 200 Constitution Ave NW Washington, DC 20210 Re: Violations of Part 7 of the Employee Retirement Income Security Act Relating to Health Plans’ Treatment of End-Stage Renal Disease Dear Assistant Secretary Borzi: On behalf of the 29,000 dialysis patients and family members that we serve, Dialysis Patient Citizens (DPC) asks that the Employee Benefits Security Administration (EBSA) investigate activities some group health plans have undertaken that we believe discriminate against individuals with [...]
Dialysis Patient Citizens Applauds Introduction of Dialysis PATIENT Demonstration Bills
Bipartisan, bicameral legislation mandating a new Medicare demonstration of integrated care for ESRD patients will help spread best practices for treating this population, says beneficiary advocacy group Dialysis Patient Citizens (DPC). “As an in-center hemodialysis patient of 41 years, I am well aware of the multiple health issues that a large percentage of my fellow patients have to cope with on a daily basis. Coordinating their care among health providers would lead to better outcomes for patients and reward providers for optimal care with fewer dollars spent overall,” [...]
DPC Participates in Home Dialysis Briefing Emphasizing Current Barriers to Treatment
Hrant Jamgochian, CEO of Dialysis Patient Citizens, participated in a congressional briefing sponsored by the Alliance for Home Dialysis on May 16th. DPC joined hip-hop artist David Rush, former U.S. Representative Karen Thurman, Larry Weisberg and Dr. Sue Quaggin to provide policymakers with policy options to improve access to home dialysis. DPC’s most recent membership survey indicated significant insurance barriers to access for home dialysis. However, the largest barrier for most patients was the lack of a care partner. The DPC survey found that while 74% of ESRD patients overall [...]
DPC Files Legal Complaint with the Office of Civil Rights over Discrimination by Blue Cross Idaho
On behalf of kidney patients nationally, Dialysis Patient Citizens (DPC) filed a legal complaint with the U.S. Department of Health and Human Services’ Office of Civil Rights citing discriminatory behavior by Blue Cross Idaho (BCI) against individuals with kidney failure, a disease which disproportionately impacts minorities. The complaint involves a new BCI policy guideline, targeting policyholders with kidney failure who need three times weekly dialysis to live. Under the policy, BCI screens policyholders with kidney failure to determine how their premiums are paid and dumps individuals who receive financial assistance from [...]
Re: Discrimination Against End-Stage Renal Disease Patients by Health Net
Janice Rocco California Department of Insurance 300 Capitol Mall Suite 1700 Sacramento, CA 95814 Mary Watanabe Department of Managed Health Care (DMHC) 980 9th Street, Suite 500 Sacramento, CA 95814 Re: Discrimination against end-stage renal disease patients by Health Net Dear Deputy Commissioner Rocco and Deputy Director Watanabe: With 29,000 dialysis patient members, over 4,000 of whom reside in California, Dialysis Patient Citizens (DPC) is the nation’s largest patient-led organization representing individuals with end-stage renal disease (ESRD). On behalf of California’s 84,500 ESRD patients, I want to [...]
DPC Hosts Successful Advocacy Day
After weeks of planning, Dialysis Patient Citizens welcomed 30 patients and family members to Washington, D.C. to meet with their legislators on a beautiful spring day in April for our annual advocacy day. As you may know, last year our advocates were snowed in so we were very grateful for the warmer temperatures this time around! The patient ambassadors who attended this year’s advocacy day traveled from 20 different states and had experience with all modalities; transplant, in-center hemodialysis, home hemodialysis and peritoneal dialysis. We were also [...]
DPC Delivers Speech on the Importance of Charitable Assistance for Insurance Premiums
For decades, dialysis patients have received financial assistance from nonprofit organizations to help them maintain their private insurance or Medigap coverage. Recently, insurers started to reject these types of payments in an effort to purge kidney patients from their health plans. Jackson Williams, DPC’s Government Affairs Director, and Deborah Darcy, Director of Government Affairs at the American Kidney Fund, presented on this issue at the National Association of Insurance Commissioners’ (NAIC) National Meeting in New Orleans earlier this month. “For nearly 20 years, the American Kidney Fund [...]
Patient Access to Electronic Medical Records: Dialysis Patients More Likely to Think It’s Important to View Their Information and More Likely to Do So at Least Once a Month
DPC’s most recent member survey asked patients their views on access to their electronic medical records to compare their opinions to those of the general public. Many physician practices that use electronic medical records make them available to their patients through secure “patient portals.” Half of dialysis patients say their main doctor gives them online access to their medical information, which is the same rate found for the public as a whole, according to a survey by the National Partnership for Women and Families. Dialysis patients are [...]
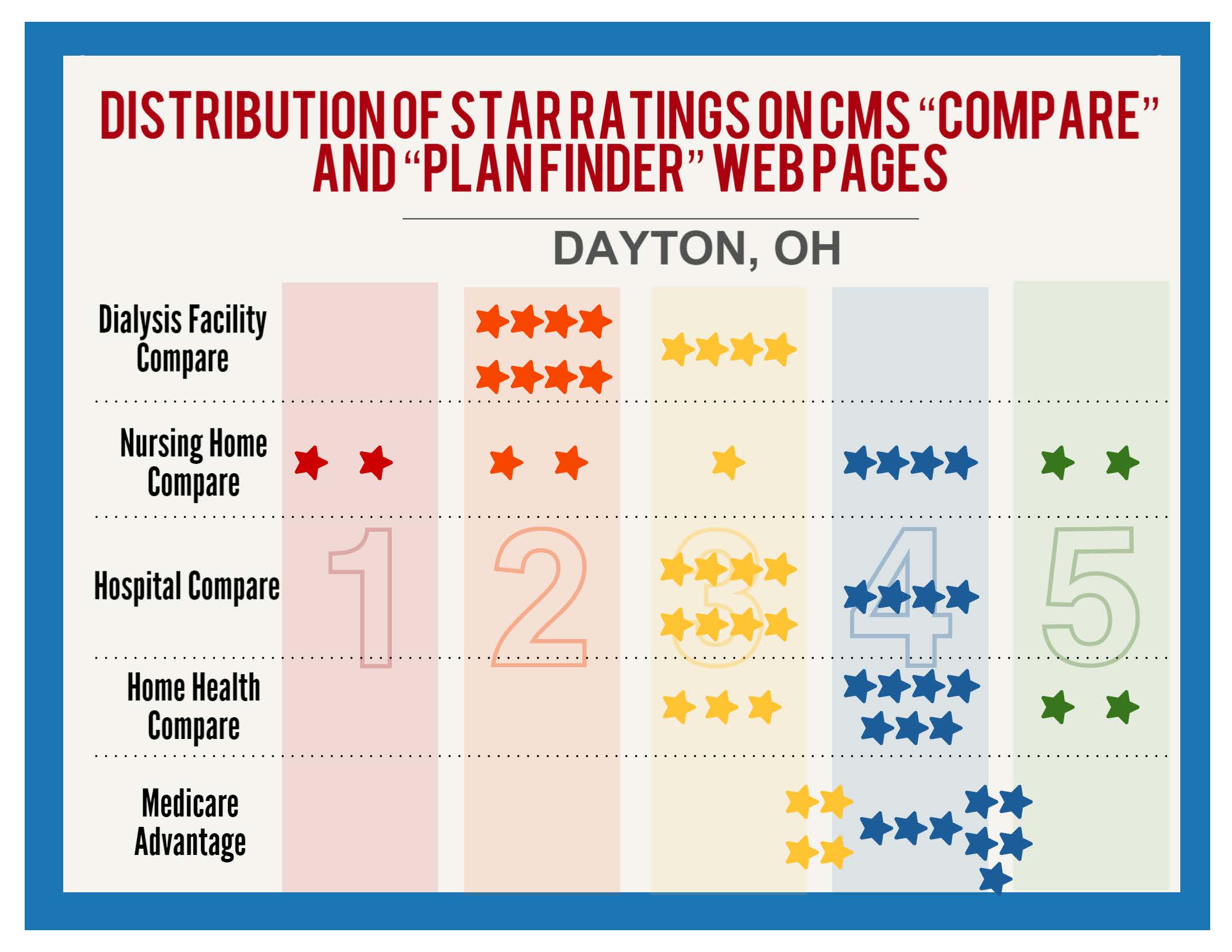
Proposed Changes to Dialysis Facility Compare Tool May Make It More Useful
Dialysis Facility Compare (DFC) is an online tool that allows users to search and compare dialysis facilities based on star ratings and certain measures. DPC has previously submitted suggestions on how to improve the proposed measures. Recently, the Centers for Medicare and Medicaid Services (CMS) announced in a Planned Changes document that the star ratings included in the DFC would be reassigned based on a 2014 threshold, meaning that the distribution of ratings would look more like it does on CMS’ other websites, and apply standards that [...]
Study: End Stage Renal Disease Patients Face Policy Barriers to Home Dialysis
Current federal policies limit patient access to home dialysis, a treatment option that offers significant clinical and quality-of-life advantages, according to a report released today by Washington, DC-based economist Alex Brill of Matrix Global Advisors (MGA). As a result of policy barriers, Brill finds a key segment of the growing population of patients who have end-stage renal disease (ESRD) miss out on the important health and lifestyle benefits of home dialysis. Brill, formerly chief economist to the House Ways & Means Committee, also finds that innovation in the [...]
Bipartisan Living Donor Protection Act Introduced to Protect Organ Donors
On February 25, Congressman Jerrold Nadler (D-NY) and Congressman Michael Burgess M.D. (R-TX), joined by Senator Kirsten Gillibrand (D-NY) and Senator Mark Kirk (R-IL), introduced the Living Donor Protection Act of 2016 to protect the rights of living organ donors. The Family and Medical Leave Act (FMLA) does not specify that living organ donors can take unpaid leave to recover from their donation and does not guarantee that donors will have a job waiting for them after surgery. Further, according to a 2007 study in the American [...]