A U.S. Supreme Court ruling has nullified the law that protects dialysis patients from discrimination by insurers, threatening the system of financing kidney care that has stood for 40 years.
The Court ruled that employer health plans may limit dialysis benefits. For four decades, employers understood the law as prohibiting limitations that only applied to dialysis. Some health benefit consultants encouraged a few small employers to disregard the law by paying no more than Medicare rates for dialysis. DaVita sued them, and one of the cases was appealed to the Supreme Court.
The decision means that employers and insurers can impose low rates for dialysis or use other benefit limitations to encourage End Stage Renal Disease (ESRD) patients to drop coverage and switch to Medicare.
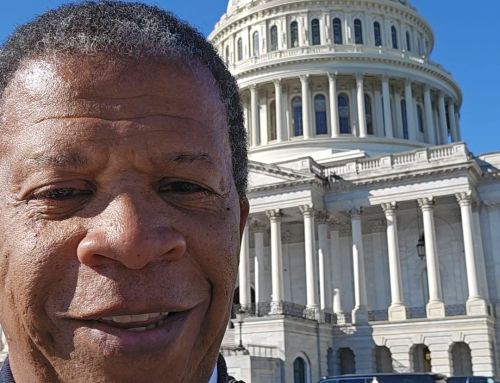
“DPC is deeply disappointed by today’s Supreme Court decision,” said DPC Board President Andrew Conkling. “Congress long ago reaffirmed privately-insured patients’ right to continue on their employer-sponsored plan for 30 months. This has played an important role in preserving patient choice and incenting plans to detect and treat Chronic Kidney Disease. To allow these plans to shift patients to Medicare before the expiration of this period represents immediate and profound risks for kidney patients and their families across the nation. As the dissenting justices stated, Congress will have to fix a statute that the Court has broken. We and other ESRD patient advocates will go back to Congress immediately to clarify the rules once and for all.”
Less reimbursement from commercial insurance means less money in the dialysis care system. This comes at a time when many health care providers are struggling to hire staff and must pay more to attract and retain workers. For many clinics, Medicare rates alone aren’t enough to break even. At best, that means fewer options for dialysis patients. At worst, communities that already have limited options and funding could have a harder time accessing treatment close to home.
The decision also weakens insurers’ incentives to detect and treat Chronic Kidney Disease (CKD) early, to extend patients’ kidney function; or to prepare CKD patients for a stable transition to ESRD.