August 27, 2025
The Honorable Mehmet Oz
Administrator
Centers for Medicare & Medicaid Services
200 Independence Avenue, SW
Washington, DC 20001
Re: CMS-1830-P – End-Stage Renal Disease Prospective Payment System
Dear Dr. Oz:
Dialysis Patient Citizens (DPC) writes to offer its comments on the above referenced proposed rule.
DPC’s membership, currently about 35,000, is restricted to kidney disease patients and their family members. DPC is a patient-led organization. Our by-laws require that the President, Vice President and at least 51% of the Board be current dialysis patients. The non-dialysis patients serving on our Board are former dialysis patients with kidney transplants. Our volunteer board members have represented their peers on CMS technical expert panels and/or advisory committees of other health care organizations such as the National Quality Forum and Patient-Centered Outcomes Research Institute. DPC also conducts periodic Membership Surveys to ascertain patients’ experiences with their care and views on health policy issues. DPC is committed to promoting access to high-quality dialysis care for individuals with ESRD; to prevention of, delayed onset of, and safe transition to ESRD among individuals with chronic kidney disease; and access to kidney transplantation as well as to other alternatives to dialysis that may emerge.
Update to the ESRD PPS Base Rate
In recent comment letters we have raised alarms about the aging-out of the health care workforce pool even as more Americans will need geriatric care. This demographic change also means that a greater share of consumers will be covered by Medicare. As such, it is critical that Medicare provider payments suffice to pay competitive salaries to frontline workers. This is especially true as the current administration attempts to restructure the workforce so more jobs are held by native-born Americans, who have been promised higher pay for traditionally low-wage work.
The past year has seen more workforce capacity warning lights blinking red:
- According to a new survey by AMN Healthcare, the average wait time for a physician appointment has dramatically increased. Across six medical specialties in 15 large U.S. metropolitan areas, the average wait time for an appointment was 31 days, up 19% since their last survey in 2022 and up 48% since their first survey in 2004.
- According to an analysis by the hospital bed company Opera Beds, more than 820 nursing facilities closed across the U.S. between 2015 and 2024, even as the over-85 population has grown by 39 percent over the past two decades.
For the ESRD PPS, the Agency is proposing an update of 1.9%. According to BLS, compensation costs for civilian workers increased 3.6 percent for the 12-month period ending in June, while inflation was 2.7%. MedPAC recently reported that dialysis clinics’ FFS Medicare margin was –1.1 percent in 2022 and –0.2 percent in 2023. They project a 2025 FFS Medicare margin of 0 percent.
We would like to bring to your attention the story of a dialysis program in southern Kansas that closed effective August 1st, just one year after it opened.
The clinic was established at Patterson Health Center in Anthony, KS after a community fundraising effort spearheaded by Harper County Health Foundation. Over $200,000 was raised from private donations, which was then matched by a grant from the Foundation. How this heartwarming project ended in heartbreak offers some lessons for Medicare ESRD payment policy.
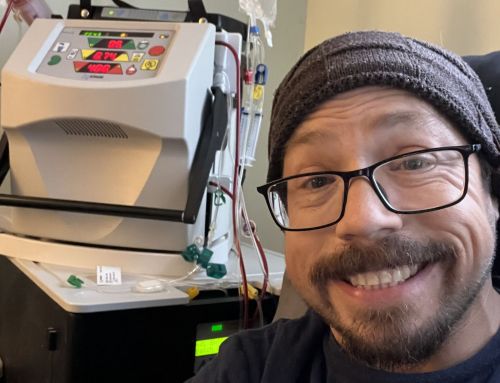
The impetus for the clinic was kidney patients and their families in this remote rural area. Funds were raised from such sources as a Dollars and Dimes for Dialysis booth at the County Fair and the Chaparral High School Class of 1973 reunion. These donations supported the purchase of three Tablo dialysis machines.
Sarah Teaff, the hospital’s director, explained the economics of trying to run a small dialysis facility on Medicare reimbursements:
Our outpatient dialysis program faced a significant financial shortfall that made continued operation unsustainable. In 2024, even with generous foundation support covering start-up costs, we still operated at a loss of approximately $161,000 in a partial year.
For 2025, projections showed annual losses between $408,000 and $544,000, depending on patient volume. Reimbursement returned only about $0.42 on the dollar, creating a shortfall of nearly 60%. That gap is simply not tenable for a rural Critical Access Hospital, especially when fixed costs remain steady regardless of volume.
Clinic leadership hoped that commercial reimbursements would make up the difference. A single patient was insured by Ambetter, an ACA marketplace insurer. But, says Teaff, they have “not paid us to date, despite our team following all necessary steps, including credentialing into their network and securing prior authorizations. We’ve submitted documentation to the state Insurance Commission in an effort to apply pressure and resolve the outstanding claims. The lack of payment from commercial payers further underscores how broken the reimbursement system is—particularly for rural providers trying to offer specialty care.”
The closest dialysis facility to Anthony is in Wichita, an hour away. Patients from other counties farther west will have to drive even longer. Some patients were already coming from 50 miles away. At the time of its closure, the program had a waiting list of over 12 people, “which is more than we could see, but every day that list gets larger and larger,” said Jason Wolff, Harper County Health Foundation President.
For the ESRD PPS, the proposed labor-related share for CY 2025 is 55.2 percent. Teaff reports that “staffing cost was approximately 70% of our operating expenses in 2024. Between the full-time RN Manager, and additional part-time Dialysis Nurse, PRN Dialysis Nurse, Dialysis Tech, Medical Director, part-time RD, and part-time social worker, we overshot our staffing budget by several thousand dollars.”
Three lessons can be learned from this experience. First, Medicare dialysis payments are insufficient to cover costs, and commercial insurers cannot be relied upon to make up the difference. Employers have already been resisting paying for their share of the kidney care infrastructure, and have been emboldened by the recent Supreme Court decision permitting them to shirk. It now appears that insurers may be joining this resistance.
Second, if there was a hope or expectation that somehow community hospitals and local philanthropic efforts could make up negative margins, Harper County shows that that is wildly unrealistic. When small rural hospitals can no longer afford to cross-subsidize maternity care, they are not going to find the dollars to subsidize dialysis. This community went above and beyond the call in raising capital expenditures, but subsidizing operating expenses was clearly out of reach.
Finally, it is patients who suffer when their choices are constrained. Stingy reimbursements mean further consolidation, and inconvenience for sick patients. It is also likely to lead to less diversity of facility ownership types, as recent development seems to indicate a retreat in not-for-profit dialysis operations.
Access to New Therapies
As we have documented previously, dialysis patients are not receiving new drugs that have been shown to reduce complications and improve quality of life. With a new Administrator having taken the reins—the first physician administrator in over a decade—staff should present policy options for mitigating the perverse incentives caused by the bundling of expensive drugs needed only by subsets of exceptional patients.
DefenCath, an innovative anti-microbial designed to reduce catheter infections, is in its TDAPA period. About 20% of dialysis patients must use a catheter for access in a given year. Fewer than 10% of eligible patients are receiving DefenCath. Due to incomplete adoption it is estimated that a dollar and some change will be added to the base rate. As we saw with Parsabiv and Korsuva, this is insufficient to bring about the widespread adoption we’d expect in the absence of a rigidly bundled payment.
Making matters worse is that DefenCath represents a classic wrong-pocket problem. A patient hospitalized for an infection means a loss of a few hundred dollars to the dialysis clinic but thousands of dollars to Medicare Part A. The misalignment of incentives practically guarantees under-adoption, greater morbidity and mortality for patients, avoidable costs to Medicare and yet another horror story to deter venture capital investments in bundled drugs. CMS can avert this by finding a way to pay separately for these products.
Quality Incentive Program Changes
The Rule proposes removal of the Facility Commitment to Health Equity reporting measure, Screening for Social Drivers of Health reporting measure, and Screen Positive Rate for Social Drivers of Health reporting measure. We did not support the addition of these measures and do not oppose their removal. However, we continue to believe that social determinants of health and health disparities are real problems faced by dialysis patients in the U.S. As we have stated before, we believe these issues should be addressed by adding resources for disadvantaged patients, not through symbolic quality measures.
The Agency also proposes cutting back the ICH CAHPS survey to 39 questions, reducing the length of the current survey by 23 questions. We have long expressed concerns about patient survey burden and declining survey response rates. This is long overdue but only a start, as the Agency must find more practical, modern, and effective ways to gather patient feedback and report it.
Thank you for your consideration of our comments and concerns. If you have any questions or would like additional information, please do not hesitate to contact me or our Vice President of Public Policy Jackson Williams (at 202-768-4506 or jwilliams@dialysispatients.org).
Respectfully submitted,
Hrant Jamgochian, J.D., LL.M.
Chief Executive Officer