By Gloria Rohrer, DPC Patient Ambassador
As a dialysis patient, it has become clear to me that one of the biggest flaws in the American health care system is the disjointed way care is often provided to patients. If patients have chronic conditions alongside other health complications, it can be exceedingly difficult to navigate the different doctors and hospitals we need in order to receive proper care.
When seeing so many different doctors at various clinics and hospitals, patients like me can suffer adverse effects if all our treatments are not designed to address our full medical history, rather than a single disease. This can be because of a lack of communication between our care providers or inadequate follow-up, which can in turn result in avoidable readmissions, medical errors or something much worse.
All of this is especially true for patients suffering from end-stage renal disease (ESRD), who often need dialysis treatment three times per week, in addition to relying on several other doctors and medications to treat accompanying health conditions like diabetes or cardiovascular disease. If an ESRD patient’s various treatments are poorly coordinated, it can lead to unnecessary and avoidable pain.
Sadly, I experienced this firsthand. My patient journey began in 1992 when my kidneys began to fail. For the past twenty-eight years, I have received treatment from countless doctors and nurses at various hospitals and dialysis care facilities.
Unlike many other cases of kidney failure, my case was unique because I did not have another underlying condition. Doctors, unable to determine what led to the kidney failure, waited before putting me on dialysis. For the next five years, I underwent weekly dialysis treatments until I finally received “the call,” or in my case, a knock on the door at 2:00 a.m. by a police officer telling me that I was going to have a kidney transplant.
Unfortunately, despite a successful surgery, three years later my new kidney failed. What followed was a long road that required emotionally and physically taxing surgeries and, eventually, the loss of my leg.
Family activities, like the vacation my husband and I took to Disney World, proved to be too burdensome. A medical emergency could not be treated at the dialysis care facility where I had planned to receive treatment in Florida, so I was rushed to the hospital.
But without a consistent coordinated care system, trips to a hospital emergency room can mean potentially dangerous treatments for dialysis patients like me. For example, nurses generally try to give us fluids as they would an average healthy adult, but for dialysis patients, that treatment can be incredibly harmful.
The lack of care coordination among facilities while in Florida left me without proper treatment and dialysis for a week. After going so long without care, pressure built around my eye and it had to be removed. While my case may just be one of many, no patient should have to share my experience.
Given that dialysis patients like myself often must see several different doctors at different hospitals, we need providers to know our medical histories to efficiently and properly treat us. The system needs to recognize that us dialysis patients have different needs than the average patient. Care coordination can offer us a more focused, personalized treatment plan that is key to a better health care system.
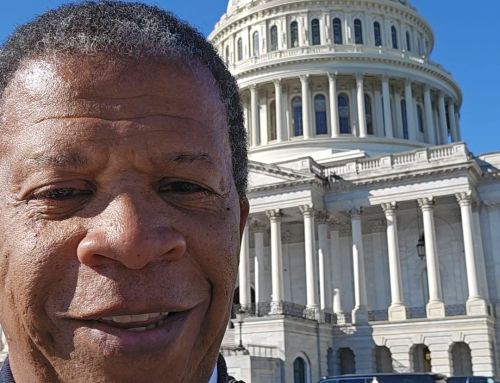
Members of Congress have already shown they acknowledge how vital coordinated care is to not just improving a patient’s treatment, but our overall quality of life. Lawmakers like Representative Jason Smith (R-MO), Representative Earl Blumenauer (D-OR), Senator Todd Young (R-IN) and others took the lead on this issue previously when they introduced the Dialysis PATIENTS Demonstration Act. They had enormous bipartisan and bicameral support, receiving more than 200 cosponsors in the House and Senate. Now Congress is positioned to take the next step in instituting coordinated quality care.
Lawmakers have made improvements on the Dialysis PATIENTS Demonstration Act with a new bill they are working on called the BETTER Kidney Care Act. It provides a coordinated care framework for ESRD patients, offering a holistic treatment plan designed to cut down on duplicative services, reduce health care costs and provide dialysis patients with the services we need but aren’t covered by Medicare, like dental care and transportation to and from treatment centers. The BETTER Kidney Care Act changes dialysis patients’ lives for the better by treating us as an entire patient as opposed to any single disease.
Legislation like the BETTER Kidney Care Act provides much-needed relief to patients like me. This kind of legislation restores confidence in medical care providers when diagnosing and administering the proper treatment. Let’s encourage our policymakers to focus on improving care coordination by supporting this bill.